Discover Our Programs
Join our diverse community of top-tier students playing active roles in their local and global communities.
View All ProgramsResearch and Innovation
In Numbers
210,000+
Citations across HBKU
8300+
Publications across HBKU
$5.9
Million dollar funds in AY22/23
346
Copyrights Protection (grants/patents)
Newsroom
When Algorithms Meet Oncology: AI’s Growing Role in Managing Breast Cancer
Breast cancer remains a major health challenge for women, being the most commonly diagnosed and leading cause of cancer death worldwide. In Qatar, it represents the highest prevalence in the overall population, accounting for 38.8% of cases in women in 2022. It is also the fourth leading cause of cancer-related deaths in Qatar. Despite major advances in treatment and the introduction of new drugs such as immunotherapy and targeted therapy, not all patients respond fully or for the long term.
Differences in how patients respond are linked to complex genetic, biological, and environmental factors that vary from person to person.
This underscores the urgent need for new analytical tools that combine different biological data to better understand why tumors behave differently in order to identify markers that help predict treatment response. Such approaches are essential for advancing personalized treatment strategies and improving clinical outcomes in breast cancer.
Integrating Artificial Intelligence (AI) and Breast Cancer Care
Advances in AI are transforming the landscape of breast cancer diagnosis and care. AI can quickly analyze huge amounts of medical data, helping doctors detect diseases earlier, choose better treatments, and improve patient care. To date, the U.S. Food and Drug Administration (FDA) has approved several AI-based tools to support cancer diagnosis, prognosis, and treatment decision support.
Breast cancer screening and early detection significantly improve treatment outcomes and recovery rates. Recent studies show that adding AI to standard screening methods such as mammography, MRI, and ultrasound helps detect cancer more accurately and at earlier stages.
In 2025, the FDA approved a novel AI-based tool, Clairity Breast, designed to analyze mammogram images and identify subtle patterns that may not be visible to the human eye. This system provides radiologists with a validated five-year predictive risk score from screening mammograms, supporting early detection. By enhancing early risk stratification, Clairity Breast aims to reduce late-stage cancer diagnoses, lower healthcare costs, and ultimately improve patient survival.
Recently, another AI-based detection tool, ProFound Detection Version 4, has received clearance from the FDA. This solution showed significant improvements in cancer detection, particularly within dense breast tissue (one of the biggest challenges in breast imaging), and reduced false positives, thus improving clinical accuracy and efficiency. Furthermore, several studies demonstrated that AI-supported double reading was associated with a higher breast cancer detection rate and specificity compared to standard double reading by radiologists, while reducing the screen-reading workload. Similarly, AI-based tools could improve radiologists’ diagnostic performance in differentiating benign and malignant lesions in breast ultrasound and MRI images. Therefore, these systems may reduce unnecessary biopsy rates while maintaining a low false-negative rate.
Patient Stratification and Personalized Medicine
AI is helping doctors personalize breast cancer treatment by combining information about each patient’s genes, health, and background to predict how they might respond to different therapies. Recently, deep learning models have been able to predict the pathologic complete response (pCR) to neoadjuvant systemic therapy (where the tumor is shrunk using several methods before surgery) in patients with triple-negative breast cancer (TNBC) based on pretreatment multiparametric breast MRI and laboratory data combined with age and gender, achieving high specificity and sensitivity.
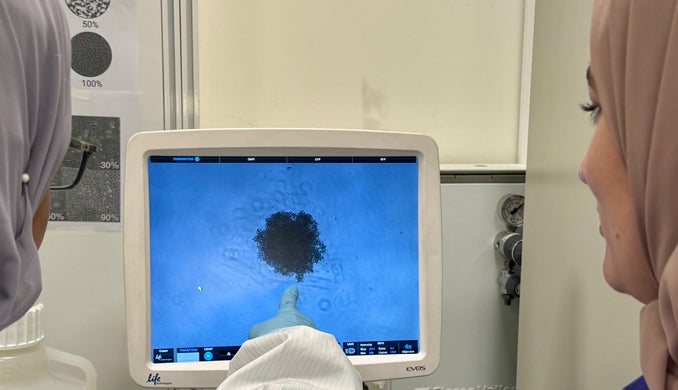
Another study reported that a combined model of clinical, radiomic (including CT, MRI and PET scans), and transcriptomic heterogeneity data (measuring changes in gene expression) from breast cancer patients receiving neoadjuvant chemotherapy achieved the highest accuracy in predicting pathological complete response. Similarly, a group of researchers developed a machine learning-based radiomics signature for estimating breast cancer tumor microenvironment phenotypes and predicting anti-PD-1/PD-L1 immunotherapy response. Researchers have developed a deep learning model that integrates next-generation sequencing data with immunohistochemistry staining images (fluorescently labeled antibodies targeting specific cancer markers in tissue) to predict response to HER2-targeted neoadjuvant chemotherapy. This model showed a strong predictive performance.
Biomarker Discoveries, Prognosis and Treatment
Finding new signs or “biomarkers” that can help diagnose breast cancer early or predict how it will develop is a complex process. In the last few decades, AI has processed an enormous amount of multi-omics data with high accuracy, which could help play a crucial role in diagnosis, prognosis, and treatment options. The technology is particularly effective at finding correlations between molecular features and clinical outcomes, uncovering biomarkers that traditional statistical methods may miss.
By enabling more accurate, personalized, and data-driven predictions of patient outcomes, AI implementation in identifying accurate biomarkers has improved the prognosis for breast cancer. Combining various data types, such as radiology scans, genetic profiles, histopathological images, and electronic health records through AI-driven models, could improve the interpretation of complex data patterns. These models frequently outperform conventional statistical techniques in predicting recurrence risk, overall survival, and disease-free survival. For instance, features such as tumor-infiltrating lymphocytes and mitotic activity – two critical prognostic indicators, can be measured using deep learning algorithms on whole-slide histopathology images. Similarly, AI models based on radio-genomics and radiomics can enhance precision medicine by non-invasively connecting imaging data to molecular subtypes and treatment responses. These models help explain how a tumor is expected to respond to various types of treatment, including immunotherapy, hormone therapy, targeted therapy, and chemotherapy.
Drug Design and Novel Therapeutic Target Identification
While AI has emerged as vital for diagnosis and treatment plans, its ability to identify previously unknown molecular pathways and biomarkers that influence tumor growth and progression makes it crucial in drug development. AI models aid in predicting drug-target interactions, identifying resistance mechanisms, and tailoring drug combinations for specific breast cancer subtypes. AI is speeding up the process of finding and testing new drugs, as well as cutting down both time and cost in developing better treatments for patients. These AI-based methods not only enhance the efficiency of drug development but also facilitate the advancement of precision oncology by enabling the creation of personalized treatments tailored to a patient’s tumor biology.
Despite these promising advances, challenges such as data privacy, fairness, and regulatory approval remain to be addressed before AI can be fully deployed in hospitals and clinics. Still, ongoing research and development in explainable AI, federated learning, and multi-modal data integration offer hope for more reliable and fair prognostic tools in breast cancer care.
Dr. Hanan Qasem is a postdoctoral researcher and Sarra Mestiri a senior research associate, both at Hamad Bin Khalifa University’s Qatar Biomedical Research Institute.
Life at HBKU
Our community embodies excellence and fosters the guiding values of leadership, innovation and discovery.
+
+