By integrating AI into the pathology workflow and leveraging advanced algorithms, clinicians can push beyond the limits of regular microscopy, enabling breakthroughs in cancer diagnosis
Breast cancer remains the most common type of cancer and leading cause of cancer-related deaths among women worldwide. The use of artificial intelligence (AI) in examining medical images, especially digital pictures of tissue samples under the microscope, is one of the most revolutionary developments in the field of medicine. These technologies promise to enhance doctor expertise, not replace them, leading to more precise classification, quicker diagnosis, and customized treatment regimens.
The Role of Emerging Technologies
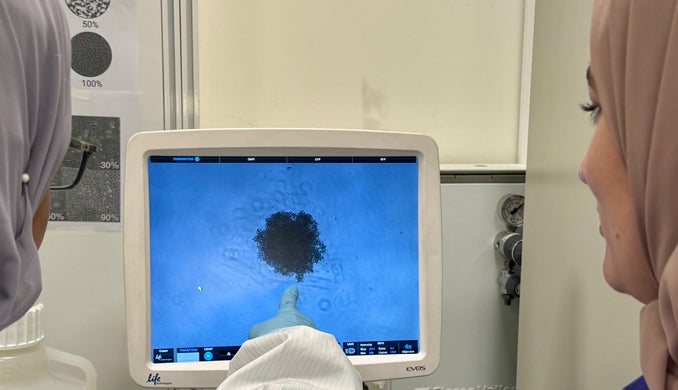
Traditionally, pathologists evaluate biomarkers, grade tumors, and interpret tissue slides depending primarily on the trained eye. Although this skill is essential, it is also limited by human capabilities such as fatigue, interpretational variations, and the overwhelming number of cases handled by the pathologist. AI and machine learning algorithms are now being developed to overcome these limitations by scanning thousands of digital images in minutes and detecting subtle details and patterns that might be missed by experienced and skilled specialists. By integrating digital slides into the pathology workflow and leveraging advanced algorithms, clinicians can push beyond the limits of traditional microscopy, enabling deeper analysis and the potential for AI-driven breakthroughs in cancer diagnosis and treatment.
Recent studies demonstrate that AI algorithms can accurately classify breast cancer subtypes and grade tumors. For example, these algorithms have an impressive ability to detect lymph node metastases, sometimes finding even tiny collections of cancer cells that might be missed during a standard review. This was demonstrated in international research projects such as CAMELYON16 and CAMELYON17, providing strong evidence that deep learning algorithms can perform as well as, and in some cases exceed, pathologists in detecting metastatic breast cancer in lymph node tissue. AI is also being developed to assess important molecular features, such as HER2 - a protein that helps guide treatment decisions for breast cancer patients - and predict how a patient might respond to chemotherapy before surgery.
In clinical practice, several digital pathology platforms have received U.S. Food and Drug Administration (FDA) clearance for use in diagnosis, marking a significant milestone toward the adoption of AI-enabled pathology platforms in the clinic. For instance, the Philips IntelliSite Pathology Solution is the first whole-slide imaging system to receive FDA clearance, enabling diagnoses to be made directly from digitized slides. Since then, other systems have entered the market, including AISight Dx (by PathAI), PathPresenter Clinical Viewer, and many others, each cleared for diagnostic purposes. These platforms often provide the infrastructure upon which AI-based algorithms for tumor detection, grading, and biomarker scoring can be deployed, paving the way for broader integration of digital pathology into everyday clinical practice.
Integrating Human and Machine
While these advances can potentially transform digital pathology, some might view them as competitors to pathologists, which is far from the truth. Pathologists must be actively involved in this process to train, validate, and contextualize AI results. Although algorithms can identify patterns, the pathologists and clinicians remain responsible for interpreting these results in the context of the larger clinical picture, combining patient history and available treatment options to provide final recommendations. By streamlining repetitive processes, like tumor grading and biomarker quantification, this joint effort enables pathologists to focus more on complex diagnostic dilemmas and direct patient care.
Despite this aspiration, several challenges remain to be addressed before AI can be fully integrated into healthcare. The quality of data used to train algorithms directly determines their performance. If training datasets lack diversity, AI risks introducing bias and producing inconsistent results across populations. In this scenario, including underrepresented populations is crucial to ensure both equity and accuracy across diverse geographic regions.
Before the widespread adoption of AI in digital pathology, regulatory frameworks, transparency in algorithm design, and robust clinical validation are essential. Moreover, many AI models function as "black boxes," producing results without explaining how, which raises concerns. Other ethical considerations, including data privacy, accountability, and the broader socioeconomic impact of AI on the pathology workforce must be addressed. Such tasks require rigorous validation of AI systems to ensure accuracy, protection of patient data, and the development of AI solutions that are fair and equitable across all populations, particularly in countries with limited financial and technological advancements.
Emerging systems aim at combining tissue images, with radiology, genomics, and other clinical data to better determine treatment response or recurrence risk more accurately than single-modality approaches. Advances in explainable AI will further improve clinician confidence. At the same time, cloud-based and federated learning frameworks can enable global collaborations by allowing institutions to jointly train AI models without sharing sensitive patient data, thereby protecting privacy. Ultimately, the vision is for AI to act as an intelligent partner to doctors across the cancer care continuum, from screening to treatment planning, helping clinicians deliver faster diagnoses, more precise treatment decisions, and improved patient outcomes.
Dr. Nehad Alajez is Principal Investigator at the Translational Oncology Research Center at Qatar Biomedical Research Institute, and Joint Professor at the College of Health and Life Sciences, Hamad Bin Khalifa University.
This piece has been submitted by HBKU’s Communications Directorate on behalf of its author. The thoughts and views expressed are the author’s own and do not necessarily reflect an official University stance.
Related News