Since the outbreak of the COVID-19 pandemic earlier this year, researchers and medical practitioners have been intensively studying the etiology of this disease and discerning its risk is population sub-groups. This week, QBRI experts discuss what is known about COVID-19 in children and how the disease can be managed in high-risk diabetic patients.
COVID-19 in Children
The COVID-19 pandemic has not been limited to adults and older members of our communities. To the contrary, reports are emerging that COVID-19 does affect children and infants and that, in some cases, serious clinical complications occur. According to current data, clinical symptoms of COVID-19 in children are milder relative to adults; some children do, however, require hospitalization and even intensive care (1-3). The Coronavirus Infection in Pediatric Emergency Departments (CONFIDENCE) study on 100 Italian children (under 18 years of age) indicated that 21% of the patients were asymptomatic, 58% had mild disease, 19% had moderate disease, 1% had severe disease and 1% were in critical condition (4). Most of the hospitalized children were found to have pre-existing medical conditions, such as lung or cardiovascular diseases, or to be immunosuppressed.
However, surprisingly, since the start of the COVID-19 pandemic, numerous reports have emerged of young patients showing multisystem inflammatory conditions with symptoms similar to toxic shock syndrome and Kawasaki disease. In Italy and France, the occurrence of this multisystem inflammatory condition has been approximately 30 times higher during the pandemic when compared to the pre-pandemic period (5, 6). The majority of these affected children are COVID-19 positive or had known exposure to SARS-CoV-2 and they have serious immunological complications requiring intensive care, indicating the potential link between COVID-19 and this multisystem inflammatory condition.
The World Health Organization (WHO) has termed such COVID-19-associated conditions as multisystem inflammatory syndrome (MIS-C) or pediatric multisystem inflammatory syndrome (PMIS) (7). Children with PMIS/MIS-C have an immunological response affecting their organs and blood vessels, and the inflammation may result in heart damage. The symptoms of PMIS/MIS-C are high fever lasting for more than five days, severe abdominal pain, vomiting, diarrhea, skin rashes, changes in skin color, difficulty in feeding/drinking/breathing and chest pain. The symptoms could also include swelling and redness of the hands and feet, redness or cracking of the lips or tongue and swollen lymph nodes in the neck.
PMIS/MIS-C is treated with intravenous (IV) immunoglobulin, aspirin and sometimes with steroids to reduce blood-pressure (8). PMIS/MIS-C occurring after COVID-19 is likely a postinfectious syndrome, meaning the patients are no longer contagious.
As COVID-19 can be asymptomatic in many children, their involvement in community-based transmission may be anticipated, especially considering that COVID-19 manifests in this age group as an upper respiratory tract infection that is more susceptible to transmission (9). Further studies are necessary to rigorously understand the short and long-term impact of COVID-19 in children to inform their management. Understanding this will be essential now as lockdown restrictions are being eased and opening schools and childcare centers are being considered.
Patient Management in COVID-19 With Diabetes Mellitus
Diabetes is among the most frequently reported comorbidities in patients with COVID-19. Indeed, diabetes is an important risk factor for mortality in COVID-19 patients. The majority of people infected with COVID-19 present with cough, fever, shortness of breath and, less commonly, nausea and diarrhea (10). When diabetic patients are infected, symptoms may initially be milder but rapid deterioration may occur in comparison to non-diabetics (11).
Upon diagnosis and assessment for the infection severity, patients with mild disease are sent for self-isolation and self-management at home with telephone follow-ups by health care personnel. With more severe disease, when there is higher risk of adverse outcomes and close monitoring of disease progress is needed, the patient is hospitalized.
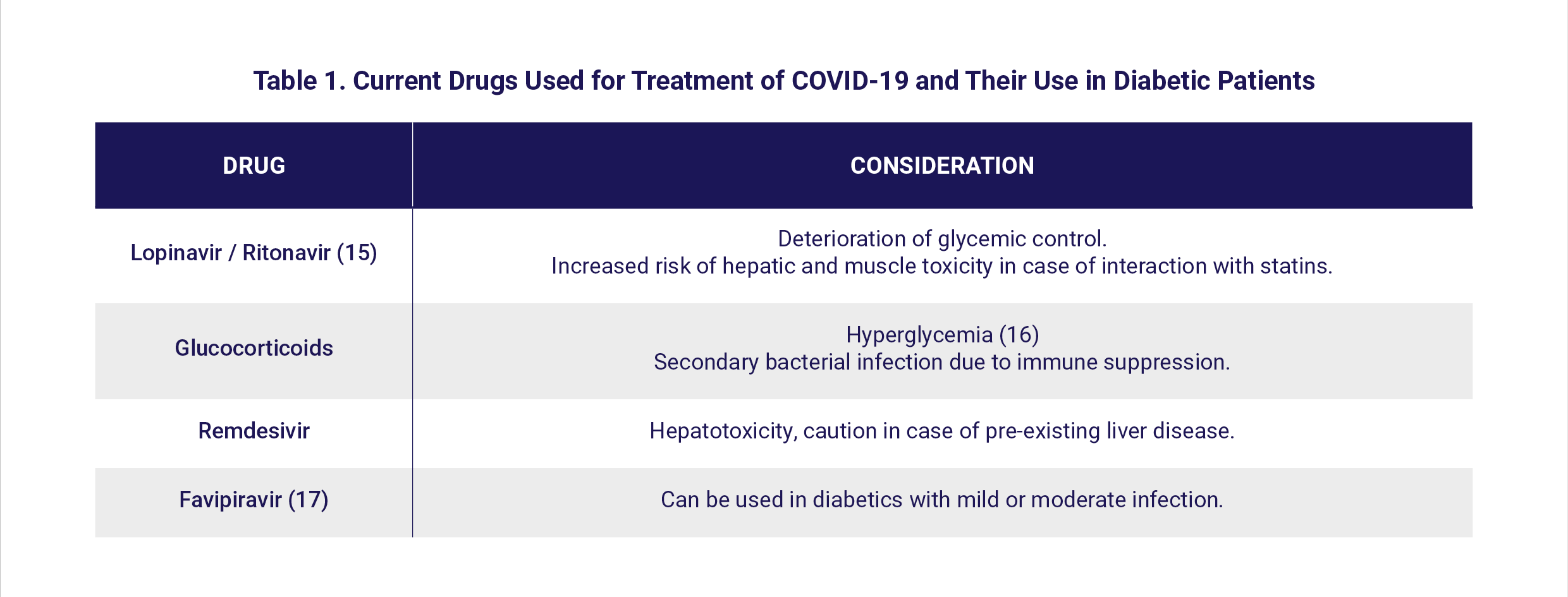
There are no definitive guidelines for the management of COVID-19 in patients with diabetes. Several drugs are being used based upon currently available clinical data; treatment decisions only weigh drug benefits against risks. Some antiviral candidates have decreased the time of viral clearance and are anticipated to show improved efficacy when used in combination with other therapeutics or antiviral agents (12). Some drugs being used in COVID-19 need special attention when used in patients with diabetes [Table 1].
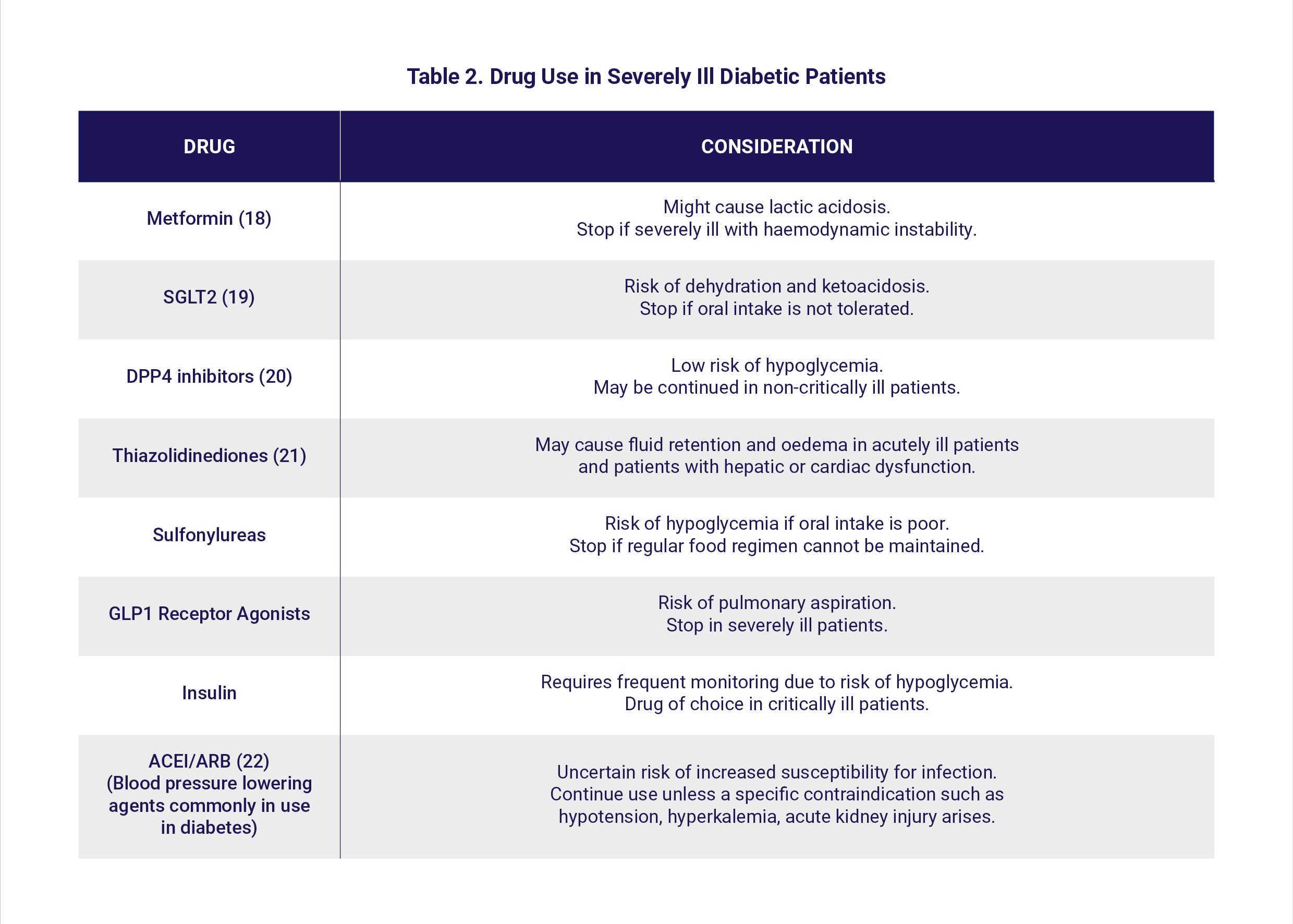
There are particular concerns regarding the use of glucose-lowering agents in diabetic patients with COVID-19. Patients with mild COVID-19 can be managed with their regular glucose-lowering agents, as long as they are able to maintain their routine eating regimen. Factors such as glycemic status, haemodynamic stability, nutritional status, renal function, risk of hypoglycemia, drug-drug interactions and availability of medications all influence the decision-making choice of drug [Table 2].
There is an increased risk of severe complications, including Adult Respiratory Distress Syndrome and multi-organ failure, in patients with diabetes (13). There is also a risk that excess fluid exacerbates pulmonary oedema in the severely inflamed lung, thus considerable care in fluid balance is required in hospitalized patients. Moreover, hypokalemia (low potassium concentration in blood), possibly associated with hyperaldosteronism (increased levels of a hormone called aldosterone) induced by high concentrations of angiotensin 2, is a common feature in COVID-19. Thus, potassium balance needs to be considered carefully in the context of insulin treatment, as it could be aggravated following initiation of insulin therapy (14).
Anti-hyperglycemic agents that can cause volume depletion or hypoglycemia should be avoided. Although there are no strict guidelines regarding insulin regimens for glycemic control in critically ill patients, intravenous insulin infusions and short or rapid-acting insulin boluses can be used.
In patients with type 1 diabetes and COVID-19 and hyperglycemia, it is important to monitor the blood glucose and ketone levels, maintain hydration and continue insulin therapy.
Healthcare systems need to assess and adopt strategies for treatment which maintain care and the supply of essential medicines for people with chronic diseases such as diabetes to reduce mortality risks.
Section Contributors:
COVID-19 in children: Dr. Vijay Gupta (Postdoctoral Researcher, QBRI)
Patient management in COVID-19 with diabetes mellitus: Dr. Manjula Nandakumar (Senior Research Associate, QBRI)
Arabic text validation: Dr. Nour K. Majbour (Research Associate, QBRI)
Editors: Dr. Adviti Naik (Postdoctoral Researcher, QBRI) and Dr. Alexandra E. Butler (Principal Investigator, QBRI)
For references, please click here.
Related News