Despite outstanding progress in the treatment of various diseases, the global burden of communicable and non-communicable diseases continues to be heavy. This burden is a major concern for economies and healthcare industries worldwide. Based on the origin or cause of the disease, its transmission or hereditability, disease development type and the treatment modalities, epidemiologists can classify a disease as communicable or non-communicable. In fact, communicable and non-communicable diseases contribute to more than 90 percent of the total global burden of disease. Idiopathic diseases constitute a third class of diseases with uncertain or unknown origins.
Classifying Communicable and Non-Communicable Diseases
Based on Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) definitions, non-communicable diseases tend to be chronic and slow-motion disorders, because of the time it takes to exhibit signs of the disease (up to one decade in duration). Additionally, non-communicable disease have a tendency to persist for long (generally more than one year). Genetic predisposition, environmental conditions, as well as nutritional, physiological and behavioral changes and ageing are all underlying factors when it comes to non-communicable diseases. According to a recent report from the WHO and the Global Burden of Diseases, cardiovascular diseases, cancer, chronic respiratory disease, dementia, liver and kidney diseases and type 2 diabetes account for 70 to 80 percent of all deaths in the non-communicable disease category.
Non-communicable diseases are neither contagious nor infectious, meaning that they do not possess the ability to be transmitted from one person to another. A large part of the burden caused by non-communicable diseases can be avoided by identifying vulnerable individuals and having them take preventive measures. These measures include early diagnosis, detection and controlling risk factors contributing to the disease, such as cessation of smoking and alcohol consumption, promoting a healthy diet and engaging in physical activity.
Conversely, communicable diseases (also known as contagious or acute diseases) start with infectious agents and can be transmitted to other people through direct or indirect contact. This is known within the scientific field as community transmission. Where animals are involved, it is known as zoonotic transmission. Other infection incidents originate from contaminated sources in our surroundings. The presence of a high load of such infectious agents in the blood or other body fluid and during pregnancy or lactation can contribute significantly to the spread of the disease. In contrast to non-communicable diseases, communicable diseases cannot be inherited through generations. Communicable diseases can also trigger an “acute response” once in the body. These responses manifest in a number of symptoms including coughing, sneezing, diarrhea, vomiting, headache, flu and fever.
Infectious agents are broadly divided into four groups: bacteria, viruses, fungi or parasites. When combined, they can compromise the lives of millions of individuals, particularly in impoverished countries. Strategies to mitigate the adverse consequences of communicable diseases include medication (such as antibiotics, anti-viral agents and vaccines) and prevention (such as good hygiene measures, confinement and social distancing).
How Does an Infectious Agent Evolve into a Communicable Disease?
The course of a disease triggered by an infectious agent involves a sequence of interrelated events, termed the transmission chain. The ability of an infectious agent to cause disease depends upon several factors that operate within a vicious cycle. These factors include, but are not limited to nature and the load of the infectious agent, individual vulnerability, the reservoir, mode of transmission, and entry and exit routes.
COVID-19: A Communicable Disease
COVID-19 originates from a virus that has been historically responsible for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 virus), and therefore classified as a communicable disease. The mechanisms underlying the pathogenesis of COVID-19 are still under extensive investigation, which means that an effective cure for COVID-19 is still not available. Preventing transmission seems to be an optimal strategy as the world waits for a possible cure.
Epidemiological studies have linked the spread of the virus to several factors including the source of infection, viral load, transmission route, and individual vulnerability. Understanding these parameters, enforcing social distancing, and stressing isolation as public health measures have led to mitigating the risk of infection.
In the early stages of virus discovery in China, the possibility of zoonotic virus transmission (from animals to humans) was considered. Observations and reports of many Chinese patients having a link to a large seafood and animal markets in Wuhan surfaced, thus creating an ideal environment for transmission of the virus from animals to humans. However, as the infection continued to spread, it became apparent that a large number of patients were never exposed to animal markets. It also became clear that human-to-human transmission occurs via different routes. Of these, COVID-19 spreads from person to person through close contact (less than 1 meter) with infected individuals. It is transmitted via respiratory secretions in the form of droplet particles (5-10 μm) or droplet nuclei (5 m) following coughing, sneezing or talking. Inhalation of these droplets leads to transmission, and so does exposure to infected surfaces such as skin, clothes and doors, where the virus can remain active for several hours and up to three days.
The ability of the virus to survive for an extended period on a variety of surfaces creates a viral reservoir. Contact with the virus becomes possible when individuals touch contaminated surfaces and transfer the virus to their hands and mucous membranes (the mouth, nose and eyes being the three main viral entry points). Physical contact with individuals who harbor the virus on their skin or clothes represents another mean of viral transmission. In addition to droplet particles, the presence of COVID-19 RNA in stool samples, tears, and saliva, urine and blood samples from symptomatically infected individuals represents a possible source of COVID-19 infection.
Large epidemiological studies documenting the possible transmission of the virus from mother to fetus during pregnancy (intrauterine vertical transmission) or during breastfeeding (perinatal transmission) are not yet available, but there are a few reports that have not found either of these potential transmission routes to be a cause of infection. These align with other medical studies that have failed to detect the virus in the amniotic fluid, umbilical cord blood or breast milk of infected mothers. However, these conclusions require further validation via large-scale cross-sectional studies. With the ongoing COVID-19 pandemic, further studies are imperative for examining the short, mid and long-term consequences of maternal COVID-19 infections on newborns. In the meantime, undertaking stringent preventative measures is very important for the protection of the mother and fetus.
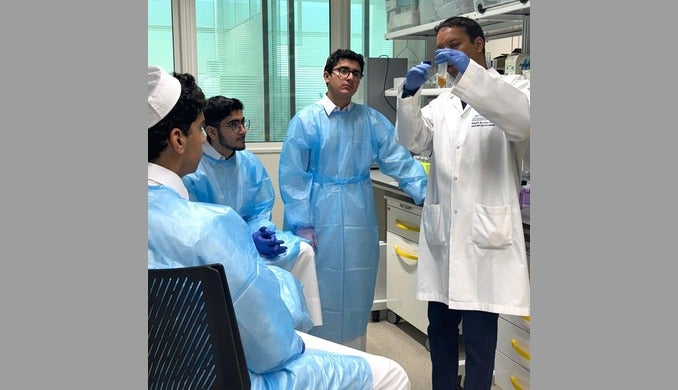
QBRI Efforts in the Fight against COVID-19
The Qatar Biomedical Research Institute (QBRI) specializes in non-communicable diseases, with a strong focus on research areas related to diabetes, cancer and neurological disorders. Yet, the institute has devoted a considerable amount of its resources and expertise towards fighting the pandemic. In a short amount of time, QBRI was able to develop a diagnostic assay to screen for individuals carrying the virus. This assay is based on real-time PCR and is now being validated. Having such setup at QBRI will greatly assists major healthcare providers in Qatar.
In addition, plans are in place for research collaborations with internal and external stakeholders such as the Qatar Computing Research Institute (QCRI), Hamad Medical Corporation (HMC), the Primary Health Care Corporation (PHCC), Qatar University (QU) and Sengenics Corporation in Singapore. Key collaborative research areas include identification of biomarkers associated with the disease, understanding the pathogenesis of the disease, and exploring therapeutic avenues based on immune response and also increasing endogenous reactive metabolite, methylglyoxal, for antiviral activity.
Contributors:
Abdoulaye Diane, Post-Doctoral Researcher
Namat Khattab, Senior Research Associate
Hanan Abunada, Research Assistant
Eman AlDous, Senior Research Associate
Alexandra Butler, Principal Investigator
Mohammed Dehbi, Principal Investigator
Diabetes Research Center, Qatar Biomedical Research Institute, Hamad Bin Khalifa University
Related News