In the midst of a global pandemic, it is important that focus on other prevalent and debilitating medical conditions, such as diabetes, is not lost. In fact, this is all the more important with diabetes, given that this disease, along with the obesity that often accompanies it, increases the risk for contracting severe COVID-19 (1, 2).
Diabetes is a metabolic disorder that represents a major medical, social and economic burden worldwide. The prevalence of diabetes has reached epidemic proportions globally, with ~425 million affected adults (20-79y), representing 8.8% of the global adult population. Current projections indicate that this figure will rise to ~629 million by the year 2045, affecting almost 10% of the worldwide adult population (3).
Diabetes is characterized by chronic hyperglycemia, a term for high blood glucose, resulting from either insufficient production of insulin by pancreatic beta-cells (type 1 diabetes, “T1D”), increased resistance to insulin action in peripheral organs (type 2 diabetes, “T2D”), or both (4-7). The pathogenesis of diabetes involves a complex interplay between behavioural, genetic, epigenetic and environmental factors (Figure 1) (8).
However, in the Gulf region, the diabetes epidemic is, in large part, fueled by obesity and sedentary lifestyles, affecting all segments of society, from the young to the elderly. Anyone can suffer from diabetes and those with affected family members are at increased risk; it is therefore critical for those at risk to follow medical advice as to the frequency of testing for diabetes.
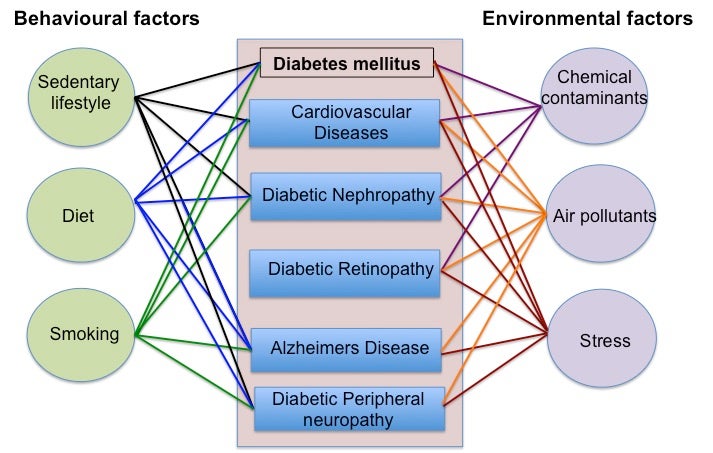
Figure 1. The complex interplay of behavioral and environmental factors that impact the pathogenesis of diabetes, diabetic macrovascular and microvascular complications and Alzheimer’s disease (a form of dementia associated with type 2 diabetes).
The devastating micro- and macro-vascular comorbidities associated with diabetes, such as retinopathy, nephropathy, neuropathy, heart disease and foot amputation/ulceration, are costly, extremely difficult to manage and lead to an increased mortality (9, 10). Diabetic patients are also at increased risk of several neurological impairments (11, 12) and certain forms of cancer (13).
Biomarkers
Fortunately, recent studies have shown that T2D can be prevented if individuals who are at risk are identified early (14). Indeed, intensive lifestyle interventions, the mainstays of which include regular exercise, a healthy diet and maintaining a healthy weight, can prevent the progression of prediabetes to T2D (14).
Prediabetes, a condition that precedes T2D, means that the glucose level in the blood is higher than normal but not high enough to be diagnosed as T2D (15). However, to identify at-risk individuals, there is a need for measurable biological characteristics, called biomarkers, that can predict the occurrence of diabetes.
This means that individuals who have the biomarkers are more likely to develop diabetes than similar individuals without the biomarkers. Individuals with these biomarkers can be enrolled into special preventive programs where they will be educated about diabetes risk and receive tailored interventions.
One focus of our research in the Diabetes Research Center (DRC) at QBRI is to identify the most accurate genetic and molecular biomarkers that are predictors of prediabetes and/or diabetes occurrence.
Targeted drug discovery and precision medicine
The underlying causes of insulin resistance leading to the development of T2D are not addressed by any current therapy. At DRC, we are investigating the mechanisms of insulin resistance to identify new targets for drug discovery. We are pursuing a recently discovered novel and safe pharmaceutical intervention that reverses insulin resistance in obesity and likely also the early stage of T2D.
There is also evidence that insulin resistance impairs lung function. This may increase susceptibility to COVID-19. So, we are exploring repurposing of a dietary supplement that corrects insulin resistance for improvement of respiratory health and thereby provides resistance to COVID-19.
In recent research, we have discovered biomarkers for assessing the risk of future decline in kidney function. Patients with diabetes may develop diabetic kidney disease (DKD) - one of the most feared complications of diabetes. Approximately one-in-three patients with T2D will develop DKD with decline in kidney function, leading to the eventual requirement for renal dialysis. With a new test using biomarker-based diagnostic algorithms, we can identify patients at risk of developing DKD in the very early stages. Guided by this, in the future, early drug treatment may maintain kidney function and prevent development of severe DKD.
Stem cell therapy
With the advent of stem cell technologies, the concept emerged of mimicking nature to generate new beta-cells to reverse diabetes, a potential cure for patients with both T1D and T2D (16, 17). Human pluripotent stem cells (hPSCs) have the potential to provide an unlimited source of pancreatic beta-cells, though much work needs to be done to allow for safe and effective therapy (17).
The ultimate goal of the stem cell program at QBRI is to pave the way for developing novel therapeutic strategies for diabetes treatment. Dr. Essam Abdelalim’s team at DRC aims to achieve two main goals: (1) understanding genetic factors underlying the development of diabetes using induced pluripotent stem cell (iPSC) technology; and (2) generation of functional insulin-secreting beta cells from hPSCs for cell therapy.
Dr. Abdelalim’s team recently established new protocols to generate pancreatic progenitors and functional pancreatic beta cells. They have also established several iPSC lines from Qatari and non-Qatari patients with different forms (monogenic and polygenic) of diabetes.
These patient-specific iPSCs can give key information about the disease pathogenesis and provide beta cells for personalized therapies. Furthermore, these models can be used for large-scale screens to examine candidate drugs that exert effects on beta cells and insulin-responsive targets. This would provide an essential platform for understanding the genetic factors of diabetes that can eventually be translated into effective treatment.
We have established national and international collaborative partnerships with Harvard Stem Cell Research Institute (HSCI), Hamad Medical Corporation (HMC), Weill Cornell Medicine - Qatar (WCM-Q), and Sidra Medicine. Also, given the groundbreaking nature of scientific research taking place at QBRI, the Qatar National Research Fund (QNRF) has actively stepped in to provide funding for several projects at the institute to help overcome the challenges often faced by laboratories in other parts of the world.
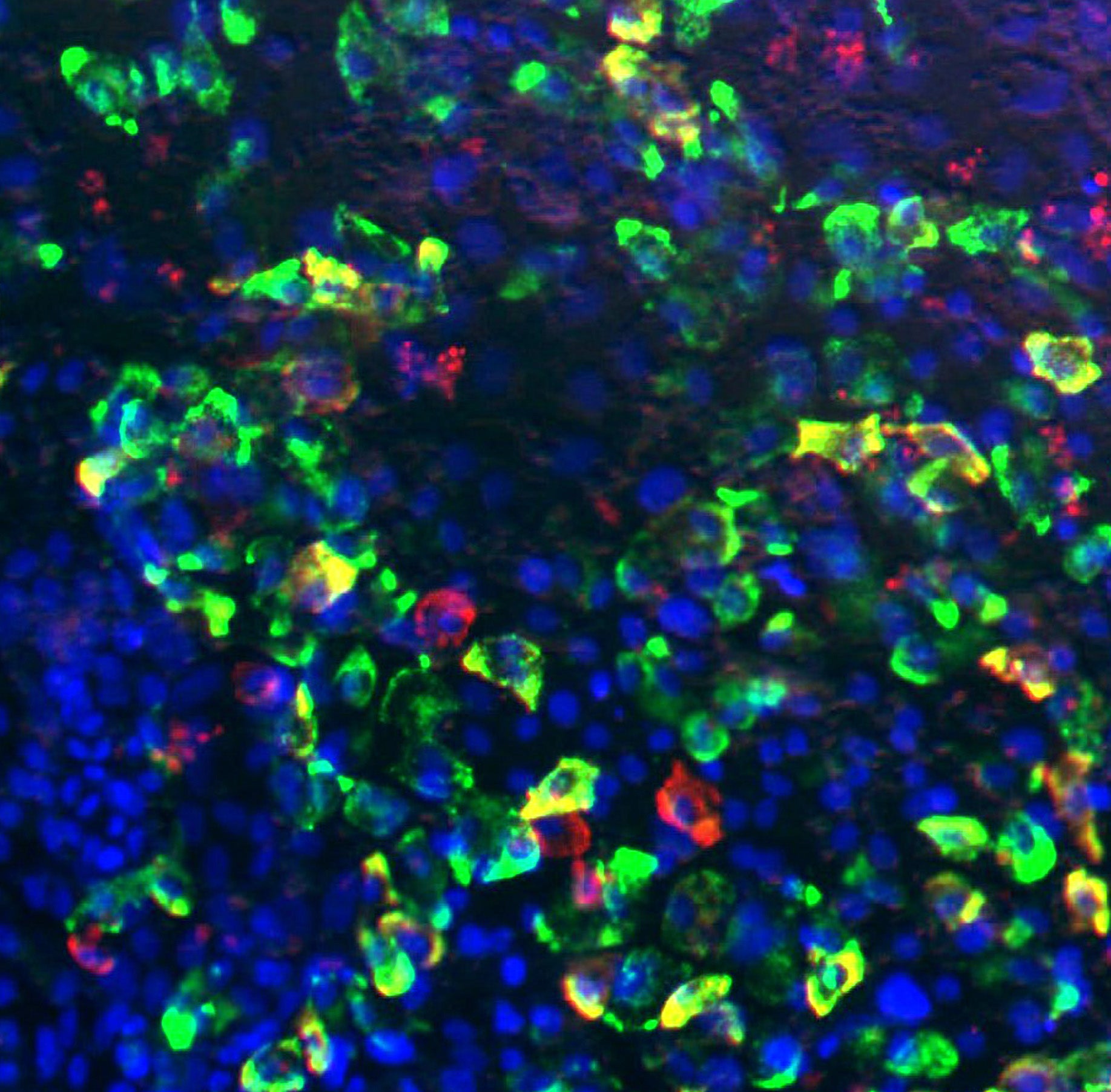
Figure 2. An image acquired using a fluorescent microscope showing the generation of islet-like cells from iPSCs (green: Insulin; red: Glucagon; blue: DAPI, that stains the nuclei of cells).
Section Contributors
Biomarkers: Dr. Abdelilah Arredouani (Scientist, QBRI)
Targeted drug discovery: Dr. Paul Thornalley (Director, Diabetes Research Center, QBRI)
Stem cell therapy: Dr. Essam Abdelalim (Scientist, QBRI)
Illustrations: Dr. Essam Abdelalim (Scientist, QBRI) and Dr. Manjula Nandakumar (Senior Research Associate, QBRI)
Arabic text validation: Dr. Heba Al-Siddiqi (Research Fellow) and Neyla Al Akl (Senior Research Associate)
Editors: Dr. Adviti Naik (Postdoctoral Researcher, QBRI), Dr. Alexandra E. Butler (Principal Investigator, QBRI)
For references, please click here.
Related News