Qatar is set to become one of the first countries to achieve mass protection in the battle against COVID-19, but what are the factors behind this success?

By Dr. Mohammad Farhan and Dr. Fadel Tissir
We are a year and a half into the SARS-CoV-2 pandemic, although mass vaccination programs initiated early this year offer hope to end the outbreak. Many countries, including Qatar and others in the Middle East, are setting their path to achieve herd immunity and restore normality through mass vaccination. Without herd immunity, the SARS-CoV-2 pandemic will revert to its original dynamic course as soon as interventions are withdrawn. The rise of new strains is an additional threat in fighting infections.
How effective are mass vaccination programs going to be?
One way to understand the effectiveness of mass vaccination is through the concept of herd immunity. Mass vaccination enhances our resistance to infection, which is how herd immunity is achieved. Indeed, when the virus meets more immunized (vaccinated) people, its chain of infections breaks, its spread halts, and gradually declines. Notably, most vulnerable individuals need to be shielded first until their regions have achieved herd immunity.
The path to herd immunity and the big difference vaccines make: The number of vaccinated and immune people needed to achieve herd immunity depends on various factors. The first factor is the reproductive virus number, known as R0, which measures how many individuals an infected individual will further infect on average. If R0 equals 1, it indicates that one infected person passes on the virus to one person on average, which means that the epidemic is stable. R0 higher than 1 suggests a surge in the epidemic and vice versa. R0 can be reduced by adhering to safety procedures such as regular hand disinfection, wearing a mask, social distancing, lockdowns, travel restrictions, and herd immunity.
Herd immunity can also be attained naturally by allowing the virus to infect a large proportion of society. Although controversial, this strategy was tested by some countries, including England and Sweden during the first wave of SARS-CoV-2 in spring 2020. However, the strategy was quickly discarded as hospitals could not handle the number of infected people who needed oxygen supply and intensive care. Further, this strategy, if allowed even in the partially vaccinated region, could be very detrimental as it provides ample opportunities for SARS-CoV-2 to further mutate and evolve to evade immunity (virus gain-of-function).
Reduction of the viral R0 can be achieved by massive vaccination. The percentage of people who need to be immunized to achieve herd immunity depends on the contagiousness of a disease. For example, the estimates for measles and polio were 95% and 80%, respectively. Most estimates have placed a threshold of 65-75% of the immunized population for SARS-CoV-2 to achieve herd immunity. However, the rise of new and more contagious strains such as the Delta variant calls for caution and a constant reevaluation. A second important factor is the movement of people in and out of the region. Maintaining restrictions on movement reduces viral R0.
Qatar has implemented many of the above measures through social distancing, making masks compulsory, implementing quarantine for travelers, and, most importantly, by vaccinating a large population in a short period.
How exactly is Qatar achieving herd immunity?
In Qatar, the government applied a stringent lockdown and mandatory mask-wearing and use of the Ehteraz mobile application to track the movement of infected individuals, plus testing in large numbers. These measures proved fruitful in preventing virus transmission and keeping the pandemic under control. Qatar started vaccinating early and shielded its vulnerable groups. Qatar has already administered 3.4 million doses of the SARS-CoV-2 vaccines. Assuming every person needs two doses, that is enough to have vaccinated about 54.6% of the population. Qatar is also one of the few countries to vaccinate its teenage population as well.
How long will SARS-CoV-2 herd immunity last?
Recent clinical trials suggest that vaccines are both safe and highly effective in preventing the most severe forms of the SARS-CoV-2 disease. However, it is still unclear how long the protective immunity will last. If the immunity duration of vaccines is similar to other coronaviruses such as MERS-CoV, a frequent vaccination of once every two to three years to multiple times in a year is needed to maintain herd immunity. The kinetics studies of antibodies generated by vaccination will help in the precise prediction of vaccine schedules. Vaccines inducing a more homogenous, uniform response in a population better provide long-duration immunity than the vaccines producing a heterogeneous response. Overall, a very high and global herd immunity threshold and adherence to social distancing and masking will be needed to prevent sustained viral spread in a population.
Does achieving herd immunity mean that SARS-CoV-2 is now no longer a threat?
Although herd immunity is protective, it is a very fragile cover, and its duration and continuation depend on various factors. Some significant factors are discussed below:
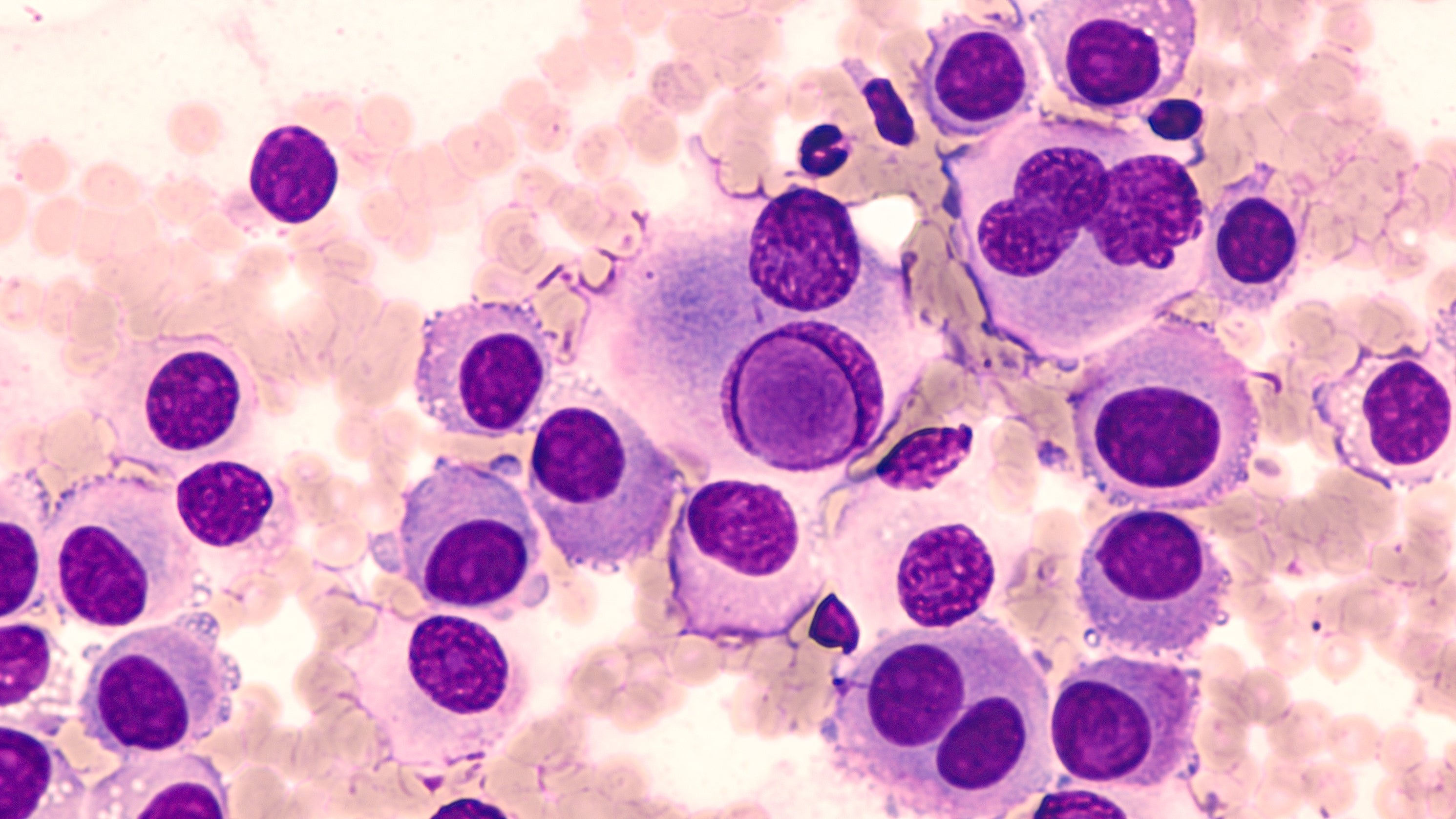
Vaccine response: A type of immunity produced by a vaccine given to a population determines how long the herd immunity will survive. The vaccine usually produces three types of immune response: production of B cells or T cells — or both. While B cells directly attack the virus, T cells target the infected cells, thus stopping virus production. While various studies indicate that vaccines produced by Pfizer-BioNTech, Moderna, or AstraZeneca-Oxford produce both B and T cell-mediated immunity, time is needed to assess whether vaccination with any of these vaccines will provide long-term immunity.
Keeping the vulnerable protected: While refusing to get a vaccine may put herd immunity at risk, some individuals may not get vaccinated because of various medical reasons like allergic reactions to the vaccine. The biggest challenge after achieving herd immunity is to keep vulnerable groups who cannot get vaccinated safe and protected from viral infection.
Testing Travelers: One of the potential herd immunity breakers or threats to herd immunity is travelers, as they can give wings to new coronavirus variants and pass it on to a population where the virus can escape the immunity, primarily through vulnerable groups. Countries need to test incoming passengers, especially those with high Infectious Disease Vulnerability Index (IDVI) scores or where new potential variants have recently been discovered. After implementing national measures designed to control the virus spread at the country level, a more global strategy should be the next step to attain worldwide herd immunity and eradicate the disease.
Dr. Mohammad Farhan (Assistant Professor) and Dr. Fadel Tissir (Professor) work at the College of Health and Life Sciences at Hamad Bin Khalifa University