By Ilham Yahya Abdi, Research Assistant

Parkinson’s disease (PD) is a neurodegenerative disorder that primarily affects movement. The disease is caused by the gradual loss of dopamine-producing cells in the brain, leading to a range of motor and non-motor symptoms. The diagnosis of PD is typically based on clinical symptoms, which include tremors, stiffness, and bradykinesia (slowness of movement). However, the neurodegenerative process of PD is thought to begin many years before these clinical symptoms emerge. As a result, there is a growing need for biomarkers that can accurately identify at-risk patients and monitor disease progression.
One promising biomarker for PD is the protein alpha-synuclein, which progressively builds up to toxic levels in the brain and spinal cord of Parkinson’s patients. Several laboratory techniques have been developed to measure clumps of alpha-synuclein in human tissues or fluids, including the cerebrospinal fluid (CSF). CSF is the liquid that surrounds the brain and spinal cord and serves as a conduit for exchanging nutrients and waste products between the brain and the rest of the body.
Two commonly used laboratory techniques for measuring alpha-synuclein in the CSF are the enzyme-linked immunosorbent assay (ELISA) and the seed amplification assay (SAA). ELISA is a fast and sensitive antibody-based approach for measuring protein levels, and it can detect the amount of alpha-synuclein clumps or oligomers. However, the diagnostic accuracy of ELISA in distinguishing PD patients from healthy controls has been unsatisfactory. On the other hand, SAA has been shown to be extremely sensitive at distinguishing PD patients from healthy people and those with other neurodegenerative conditions, potentially allowing for a definitive diagnosis. SAAs assess a protein’s seeding activity, or the rate at which a protein clumps together to form toxic aggregates.
SAA is a technique used to detect small amounts of certain proteins that are linked to some diseases that affect the brain. These proteins can be difficult to detect, but SAA is a very sensitive test that can find them even if there are only tiny amounts present in a sample. In the studies of PD, alpha-synuclein is the target protein. The way SAA works is by taking a small amount of a sample that may contain the alpha-synuclein, and then adding it to a larger volume of a synthetic alpha-synuclein that can turn the protein into a clumped form, which is called an "aggregate." These aggregates can then serve as a template to make more protein clumps, and the process can be repeated multiple times to get more and more clumps. This way, even a small amount of the target protein can be amplified and detected.
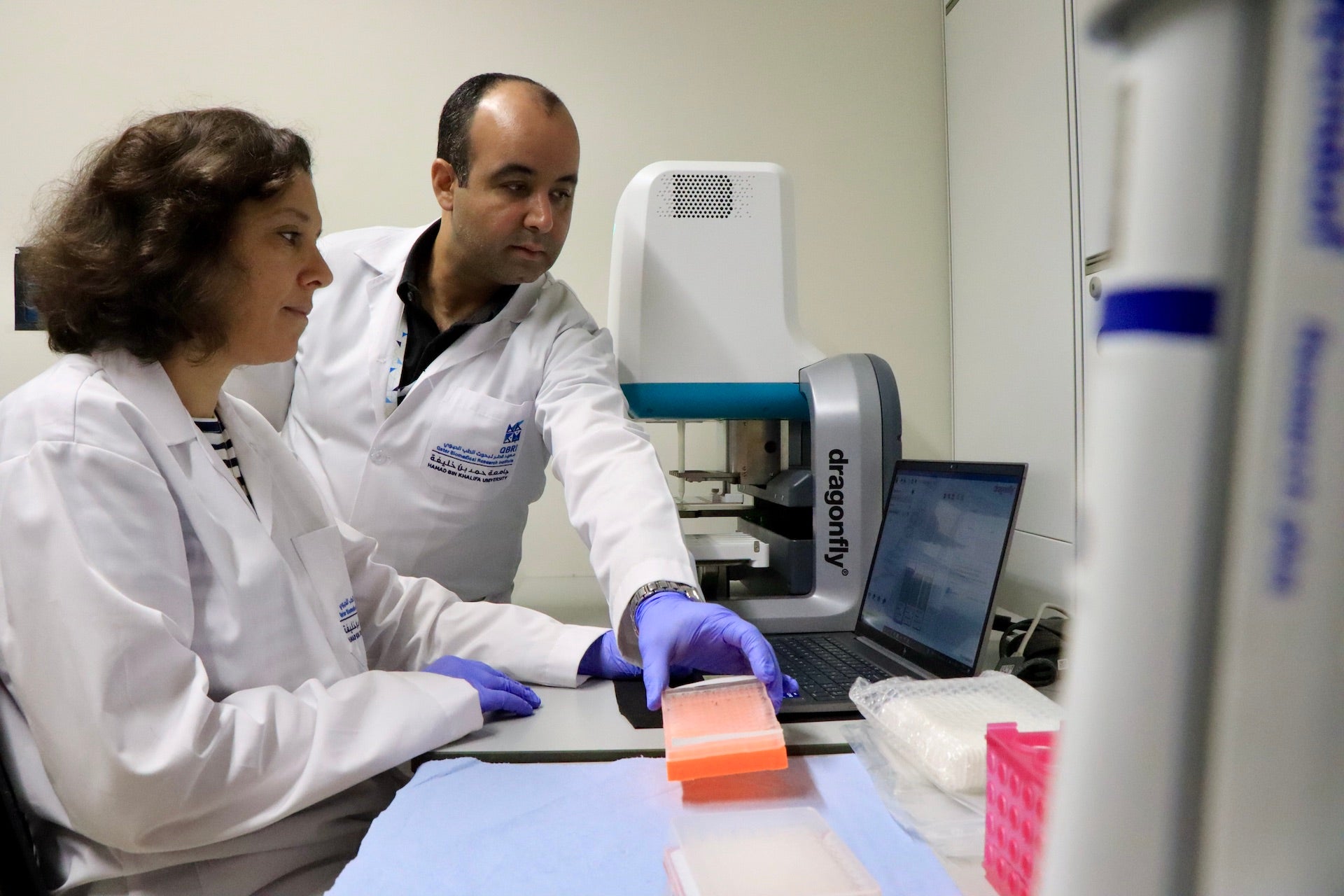
In a recent study published in Neurology titled “Disease-Associated α-Synuclein Aggregates as Biomarkers of Parkinson Disease Clinical Stage”, a QBRI research team led by Dr. Omar El- Agnaf, Principal Investigator, Neurological Disorders Research Center, investigated whether a combination of ELISA and SAA could provide a more accurate readout of CSF alpha-synuclein clumps that could reflect disease severity in patients. The approach used SAA to sensitively identify the presence of misfolded alpha-synuclein clumps, which could then be accurately quantified by ELISA.
The researchers first explored the test’s potential in brain tissue from people with PD, dementia with Lewy Bodies (DLB), Alzheimer’s disease (AD), and from healthy people who served as controls. PD, DLB and AD are all neurodegenerative diseases, but only PD and DLB is marked by alpha-synuclein buildup. The combined approach demonstrated high sensitivity in distinguishing between PD and DLB patients from AD patients and healthy controls and enabled earlier detection of the aggregates compared to using SAA alone.
The team analyzed cerebrospinal fluid samples from 62 individuals with PD and 34 healthy individuals of a comparable age to assess the diagnostic accuracy of the combined test. The results demonstrated that the test could effectively distinguish between those with and without PD. Moreover, the levels of alpha-synuclein aggregates, which were measured using the combined approach, were significantly associated with the severity of PD, as measured by the validated Unified Parkinson's Disease Rating Scale-Part-III and the Hoehn and Yahr scale. To confirm these findings, a second group of CSF samples from 49 PD patients and 48 age- and sex-matched healthy individuals was analyzed, which revealed a similar association between the combined test readout and disease severity.
The results suggest that the combined ELISA-SAA test is a valuable tool for detecting Parkinson's disease and assessing its severity, and may have potential in clinical trials targeting alpha-synuclein aggregates in Parkinson's patients. Further investigations should evaluate the applicability of this combined approach in other alpha-synuclein-related diseases and testing of therapies that target protein aggregation.
The full study can be accessed at: https://pubmed.ncbi.nlm.nih.gov/36096686/
Related News
Extensive Collaborations and Unique Technical Capabilities Unveil Neurological Protein Signature of Severe COVID-19

Advancements in Type 1 Diabetes Treatment: FDA Approves CellTrans' Lantidra Cell Therapy

Landmark Study by QBRI Unveils Impact of Cholesterol on Neurodegenerative and Neurodevelopmental Disorders